Electronic cigarette (ECig) use among adolescents poses significant public health risks. This guide provides concise, evidence-based information for practitioners.
Understanding the Appeal and Risks
Adolescents are attracted to ECigs due to flavors, perceived safety versus smoking, discreetness, and social media influence. However, nicotine exposure during adolescence:
- Harms Brain Development: Nicotine disrupts synaptic pruning and maturation in the prefrontal cortex, impacting attention, learning, impulse control, and mood regulation.
- Creates Addiction: Adolescent brains are more susceptible to nicotine dependence, often established faster and with lower exposure than in adults.
- Increases Risk of Other Substance Use: ECig use is associated with subsequent initiation of combustible tobacco and other substances.
- Causes Respiratory Issues: Even without nicotine, inhalation of aerosols containing ultrafine particles, volatile organic compounds, and flavorants like diacetyl causes airway irritation and potential long-term harm.
- Exposes to Toxicants: Contaminants (e.g., heavy metals from coils, carcinogens like formaldehyde under high heat) pose health risks. Accidental nicotine poisoning via ingestion of liquid is also a danger.
Effective Screening and Intervention
Universal Screening: Routinely ask all adolescents about tobacco/nicotine use, including ECigs (“vaping,” “JUULing,” “pods”). Use non-judgmental language: “Many teens try vaping. What have you heard about it, or have you tried it yourself?” Include screening for secondhand exposure.
Brief Intervention Strategies:
- Motivational Interviewing (MI): Emphasize autonomy. Explore pros/cons they perceive, provide personalized health information, evoke change talk.
- Clear Health Information: Specifically state the risks to their developing brain and potential for lasting addiction. Debunk “safer than smoking” myths relevant to youth non-smokers.
- The 5 R’s: Relevance (personalize risks), Risks (acute & long-term), Rewards (benefits of quitting), Roadblocks (identify barriers), Repetition (discuss at every visit).
- Ask-Tell-Ask: Ask permission to give advice (“Can I share some key health concerns about vaping?”), Tell succinct information, Ask for their thoughts/reactions.
Addressing Quitting: Offer support to those using. Adolescents experience withdrawal symptoms. While FDA-approved cessation medications are not specifically approved for teens, some evidence supports NRT or bupropion. Referral to specialized programs (e.g., state quitlines like 1-800-QUIT-NOW), counseling, or reputable digital tools is crucial. The ask-advise-refer model is practical.
Vital Role of Parents and Community
Parental Counseling:
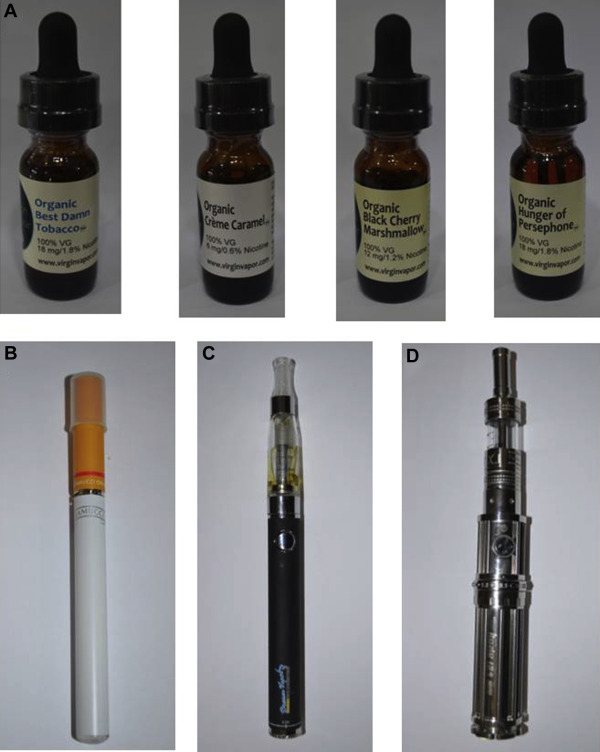
- Educate parents on ECig appearance (often disguised as USBs or pens), common slang (JUUL, puff bar, mod), signs of use (sweet smells, increased thirst/nosebleeds, discarded pods/devices).
- Encourage clear home rules against all tobacco/nicotine use. Discuss consequences, emphasize health reasons.
- Advise parents to talk openly about risks using credible resources like the FDA’s “The Real Cost” or CDC websites.
Community Advocacy: Support policies enforcing age 21 sales (T21), restricting flavored products (major driver of youth use), comprehensive smoke-free/vape-free laws, taxation, and funding prevention programs.
Key Resources
- Clinical Practice Guidelines: AAP policy statements on ECigs.
- Surveillance Data: CDC National Youth Tobacco Survey (NYTS).
- Cessation Support: Smokefree Teen resources, Truth Initiative, State Quitlines.
Sustained vigilance, screening, tailored intervention, and community efforts are paramount in protecting adolescents.










